

Partnering to Find Medication Access Paths: Todd's Story
“You're playing beat the clock with this disease.”
In these featured stories of the 2022 Medication Access Report: Oncology Edition, we explore how people living with cancer navigate their care journeys through medication access, affordability and adherence challenges in partnership with their care teams.

Read the full 2022 Medication Access Report: Oncology Edition to deep dive how technology can help with medication access, affordability and adherence challenges in the oncology space.
About one in five U.S. adults identify as unpaid caregivers to an adult friend or family member.Caregiving in the United States 2020, AARP, National Alliance for Caregiving, 2020 For some patients, caregivers can help support the cognitive load of healthcare as much as the clinical, especially when it comes to cancer care. Such is the case for Todd and Diane, a married couple from California who partner in managing Todd’s multiple myeloma, a cancer of the plasma cells.
For Todd and Diane, care management is a combination of various tactics. These include medication, advocacy work and a dogged effort to find the latest breakthroughs on the way to a cure.
While they navigate challenges in accessing Todd’s necessary medications, they also support those newly diagnosed with multiple myeloma in finding their own paths to getting necessary medications sooner. It’s needed guidance: In a recent survey, 49% of people with cancer said they’ve experienced a delay in receiving their medication.CoverMyMeds Oncology Patient Survey, 2022
“Patients need early access,” Todd said. “You’ve got to have access to (medications) to be around for the innovation that will ultimately be coming for a cure.”

After Todd was diagnosed in 2017, he and Diane knew they needed a provider who stayed abreast of cutting-edge treatment strategies for multiple myeloma. Todd and Diane continue to celebrate his ongoing remission thanks to his personalized treatment plan that includes just such a strategy. Todd takes a drug that is not yet FDA approved for multiple myeloma, but is recommended for Todd’s specific genetic makeup by clinically trusted guidelines. This isn’t uncommon — some estimates show 30% of cancer therapies are used off-label, and use could grow as the drug pipeline continues to include multi-indication therapies.Oncologists' Off-Label Prescribing Pits Access Against Reimbursement, Medscape, 2018
“You're playing beat the clock with this disease,” he said. “When there is no cure, you’ve got to stay very current on the science.”
After starting treatment, undergoing radiation and a stem cell transplant, Todd is now on maintenance therapy. That includes monthly injections, weekly steroids and daily targeted therapy, along with a host of supplemental treatments. Some studies estimate people with cancer take an average of five prescription medications.Use of Prescription and Non-Prescription Medications and Supplements by Cancer Patients during Chemotherapy; Questionnaire Validation, Hanigan et.al., 2009 It’s likely each of these can come with high costs, time-consuming access and approval processes or a complicated route of administration — or some combination.Use of Prescription and Non-Prescription Medications and Supplements by Cancer Patients during Chemotherapy; Questionnaire Validation, Hanigan et.al., 2009 That’s a lot to keep track of in addition to scans, appointments and, most importantly, life outside cancer treatment.


Read more about solutions to help care teams overcome access challenges such as utilization management for cancer medications in the full 2022 Medication Access Report: Oncology Edition.
On top of all that, Diane’s also coordinating care for her parents, who see 10 different doctors, have data on three different patient portals and labs on another two portals. Though everything is electronic, this is an example of the need for interoperability in healthcare, to improve continuity of care and reduce the information burden on care teams and caregivers.
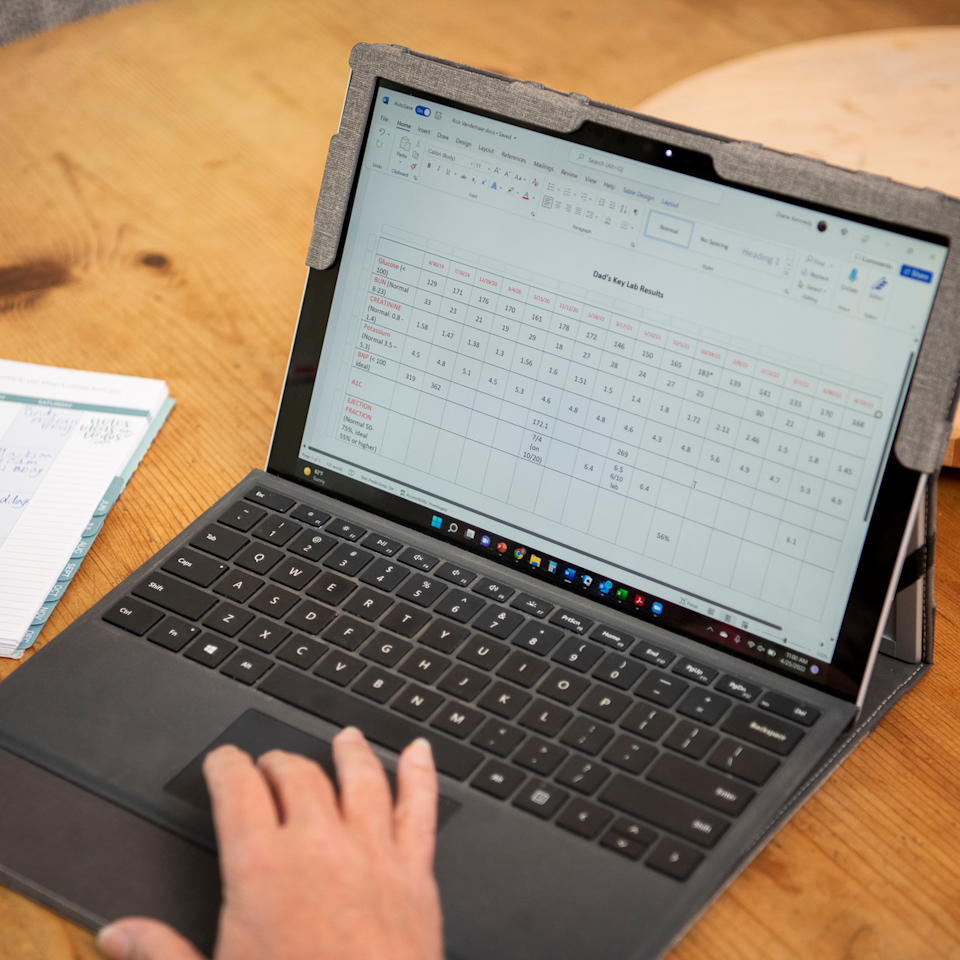
It’s no wonder Diane keeps spreadsheets and charts for Todd and her parents. Despite the disparate systems, she finds patient portals helpful with information gathering, and both she and Todd receive any scan or lab results instantly to their smartphones.
Though everything is electronic, this is an example of the need for interoperability in healthcare, to improve continuity of care and reduce the information burden on care teams and caregivers.
“I'll get pinged that the notice is in and we both race to see who’s fastest getting to the results, to see those numbers,” Diane said.
Who wins?
“She does,” Todd said with a smile. “Barely.”
While some information is easily received and tracked, other pieces — such as benefit coverage and out-of-pocket cost — aren’t so accessible. These discrepancies often start at the point of prescribing, where the potential for patient engagement is high but information to hold productive conversations is often lacking.
In a recent survey, only 49% of providers said they had the necessary benefits information to start patients on specialty therapies.CoverMyMeds Provider Survey, 2021 Without this information, providers are left to make decisions without patient-specific information. And in some cases, the burden falls on patients to track down cost and coverage information.

Diane said she’s experienced providers avoiding ordering necessary treatments because they assumed insurance wouldn’t cover the cost.
“I'd rather you make the decision based on what you need to do for the best medical care for me or my family,” she said.
Many patients seem to agree with her sentiment. When asked what characteristics are most important when considering a medication to treat cancer, patients ranked effectiveness and provider preference highest, above out-of-pocket cost and insurance coverage.CoverMyMeds Oncology Patient Survey, 2022
Solutions that electronically connect to patient-specific benefit information can help patients receive the best treatment possible and understand how to access and afford it. Workflow-integrated technology can help perform benefit checks, expedite the prior authorization process and enroll patients in hub programs in a single platform. These solutions have been shown to help patients access medications eight days sooner, on average.CoverMyMeds data on file. Case study of AMP programs analyze from APR 2019 – NOV 2021, comparing phone and fax method to electronic.
Integrated technology can also help improve transparency and communication among multiple providers and care team members. Todd plays the role of messenger between his internal medicine doctor and his oncologist, updating each on the other’s recommendations for his healthcare.
“There’s definitely a responsibility that I have to bridge that for both of them, and I wish that wasn't necessarily my role,” he said. “It’s still too siloed, even though the data is becoming much more integrated and accessible to them.”
Data flow further becomes a complication when it comes to managing medications prescribed by different providers. This is where pharmacists and specialty pharmacists serve a critical role in helping people living with cancer manage their treatment regimen. Diane and Todd both credited a specialty pharmacist for helping them know whether a new migraine medication would have a negative reaction in the body when taken with his current medications for cancer.
“That made me feel much more confident and also like we have a comprehensive, coordinated approach going here,” Todd said. “The pile of pills I take every day is so amazing. All patients need to be aware of not only what each pill does, but what they do when they're used together.”
Another thing Todd and Diane advocate for patients is searching for programs to help afford their medications. In one survey of patients on specialty medications, 40% were unaware of financial support services available to them.CoverMyMeds Patient Survey, 2019 Todd knew about patient assistance programs from his biopharma background — he just assumed he would never qualify. After encouragement and help from a pharmacist, he discovered he did qualify and now saves thousands of dollars on his medications each year.
“(Multiple myeloma) is a very expensive disease, and despite the fact that there is no cure yet, I plan to live hopefully for decades,” he said. “Every little bit helps, no matter what your financial status is.”

Affordability assistance can further help patients when it comes to adherence. In a recent study of patients prescribed oral anticancer medications, patient abandonment increased with out-of-pocket medication costs. Nearly one-third of patients didn’t fill their prescription when costs were between $100 and $500.The Pharmacoeconomics of Oral and Self-Administered Cancer Treatments, Doshi et. al., 2018 One in 8 patients in the study had prescription out-of-pocket costs over $2,000, and 49% of them never filled their prescriptions.The Pharmacoeconomics of Oral and Self-Administered Cancer Treatments, Doshi et. al., 2018
Todd and Diane continue to coach and advocate for those living with cancer and caregivers through online patient support groups and their local health system. It’s a full-time post-retirement job that Diane said jokingly can add up to more weekly hours than she worked before retiring. For Todd, the effort is worth it.
“These are highly rewarding passion projects for us,” Todd said. “It serves me personally, but it also serves others in a big way.”

Finding Affordability in Oncology Medications: Jeannine’s Story
“If I don't have those meds, what does that mean for me? ... It's very scary.”
In these featured stories of the 2022 Medication Access Report: Oncology Edition, we explore how people living with cancer navigate their care journeys through medication access, affordability and adherence challenges in partnership with their care teams.

Read the full 2022 Medication Access Report: Oncology Edition to deep dive how technology can help with medication access, affordability and adherence challenges in the oncology space.
Jeannine is living with metastatic breast cancer. To be more accurate, for the first time since her cancer diagnosis in 2019, Jeannine has begun to live again.
After going through an initial period of shock and denial, Jeannine accepted her diagnosis and began treatment, though she described her first two years post-diagnosis as “robotic.”
“It became a fog to me,” she said. “I just followed one appointment after the next appointment … until there were two years of appointments.”
During this time, Jeannine was juggling a full-time job and attending graduate school at the height of her career, emotional stress from her diagnosis and cancer treatment side effects. The pains and aches caused by one of her medications became so bad at one point, she stopped taking the medication. Side effects can be a major factor in nonadherence for cancer patients. One in 5 cancer patients surveyed who said they’ve failed to take their medications as prescribed blamed unpleasant side effects.CoverMyMeds Oncology Patient Survey, 2022

After over a year of working through treatment, Jeannine reflected on her values and what she wanted her life to look like. She was certain her new life vision didn’t include working at her IT job. Unclear, though, was what quitting her job meant for affording her cancer treatment. With one of her medications costing nearly $16,000 per dose, Jeannine knew she had to find a way to pay for her treatment and still lead the lifestyle she wanted.
Financial hardship for cancer patients, sometimes referred to as financial toxicity, is sadly a common thread. The high costs of treatment and tests can be layered on top of possible lost wages or fringe costs such as childcare or transportation. Eighty-nine percent of patients surveyed had to make life changes associated with cancer or cancer treatment, such as quitting their job, relocating or sacrificing essential items or bills.CoverMyMeds Oncology Patient Survey, 2022 One study found cancer patients face a 2.7 times greater likelihood of bankruptcy than those without a history of cancer.Washington State cancer patients found to be at greater risk for bankruptcy than people without a cancer diagnosis, Ramsey et. al., 2013

“Now I'm dealing with the stress of trying to get patient assistance to continue my medications because that's my lifeline,” she said. “If I don't have those meds, what does that mean for me? If I don't get another job within the next two or three months ... what does that mean to me? What does that mean for my health? It's very scary right now.”
Read more about how affordabilty challenges affect people living with cancer on a broad scale and solutions for care teams to help overcome these in the full 2022 Medication Access Report: Oncology Edition.

Two months later, Jeannine found help and hope
CoverMyMeds followed up with Jeannine two months later in another interview and asked about her access and affordability options for her medications since resigning from her job.
“The consideration with handing in your resignation is whether you're going to be able to afford your medications,” Jeannine said. “But I still made the decision to resign. I just went on faith.”
Jeannine took fate into her own hands and asked her provider about affordability options. Together, they applied for patient assistance programs through biopharma companies for two out of her three medications. Jeannine received approval and now pays no out-of-pocket expense for these medications. With these savings, the out-of-pocket cost for the third medication is manageable.
“It's very important to me as a patient to have available ways for me to purchase medications,” she said. “If I was on insurance, everything would be fine — but that's not what I decided to do. I wanted to do something different.
“If I did not know about the programs I applied to, that would be a huge disservice to me and my health.”

Care teams, enabled by integrated solutions, can help patients find affordability programs such as copay assistance from biopharma companies, patient assistance programs, nonprofit foundations and even cash options. They can also impact adherence — a growing concern in the cancer community as more medications are patient-administered.
In one study of cancer patients, nearly one-third didn’t fill their prescription when out-of-pocket costs were $100 to $500.The Pharmacoeconomics of Oral and Self-Administered Cancer Treatments, Doshi et. al., 2018 For patients whose out-of-pocket costs exceeded $2,000, 49% never filled their prescriptions.The Pharmacoeconomics of Oral and Self-Administered Cancer Treatments, Doshi et. al., 2018
Electronically connected solutions in provider workflows can help surface available affordability programs at the point of prescribing. This can help care teams avoid time spent searching and manual back-and-forth processes if programs were found later. It can also help pharmacists apply savings for patients at the time of pickup, further helping make sure they can start therapy sooner. Solutions that help connect patients to affordability options can impact adherence and outcomes later in the treatment journey.
In one study of patients taking oral anticancer medications, progress was significant. Patients with copay assistance had nearly $2,000 lower out of pocket costs, picked up their prescriptions 22 days sooner and had a 24% lower risk of discontinuing treatment compared to patients without copay assistance.The impact of copay assistance on patient out-of-pocket costs and treatment rates with ALK inhibitors, Seetasith et.al., 2019

In-workflow solutions also allow care teams the opportunity to engage patients in shared decision-making around their treatments. That way, they can find the right, unique path forward, inclusive of any social or personal considerations that could impact access to medications.
For Jeannine, finding easy ways to access and afford her medications has allowed her to expand and redesign her new life, beyond the constraints of a cancer patient. She’s picked up her hobbies of walking and exploring the outdoors again in a new state and has even found a new career path that allows her to give back to the cancer community.
“I have my peaks and my valleys,” she said, “days where you ask, ‘Why?’ And you may not get the answer. You may never get the answer, but I've learned to live now. Two years after diagnosis was a fog for me. I didn't know how to live. Now, I'm learning how to live.”

















